Abstract
Background: Haploidentical hematopoietic cell transplantation (haploHCT) is an attractive option for patients, who have no suitable matched-related or -unrelated donor. While the increased alloreactivity of haploidentical grafts enhances graft-vs-leukemia effects, it also increases the risk of acute graft-vs-host disease (aGVHD). Therefore, extensive in vivo or ex vivo T-cell depletion is required to reduce the incidence of severe aGVHD. However, global T-cell depletion is associated with delayed immune recovery, serious viral infections, and relapse. To overcome this limitation, selective TCRɑß and CD45RA T-cell depletion was developed. Both aim to remove alloreactive T-cell subsets, and initial clinical experience has demonstrated the feasibility and safety of each individual approach. We reasoned that combining both approaches might further increase immune reconstitution and bolster graft-vs-leukemia effects. We therefore designed an early phase clinical study, NCT02790515, to evaluate the safety and efficacy of infusing two haploidentical allografts, one TCRɑß T-cell depleted and one CD45RA T-cell depleted, in pediatric patients with very-high risk hematological malignancies, who had recurrent disease after a previous allogeneic HCT.
Methods: Patients received their second (n=16) or third (n=2) allogeneic HCT utilizing TCRαβ-depleted and CD45RA-depleted haploidentical donor progenitor cell grafts following conditioning with rabbit ATG (5mg/kg), fludarabine(150mg/m2), cyclophosphamide(60mg/kg), thiotepa(10mg/kg), and melphalan(120mg/m2) on an IRB and FDA approved single institution protocol. Tacrolimus (n=5) or sirolimus (n=13) was given for post HCT GVHD prophylaxis. At the time of HCT, 6 patients remained refractory with active disease and 9 more were in morphologic remission but had detectible minimal residual disease (MRD).
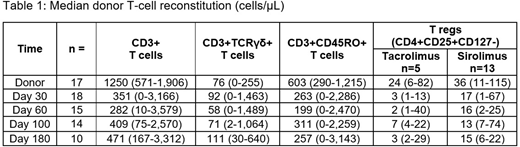
Results: The conditioning regimen and progenitor cell infusions were well tolerated without dose limiting toxicities. Patients received a median T-cell dose of 11.9x106/kg (including 0.01x106 TCRαβ T cells/kg; range: 0.00-0.09) with the TCRαβ-depleted graft, and a median T-cell dose of 50.3x106/kg (including 0.00x106 CD45RA+ T-cells/kg; range: 0.00-0.02) with the CD45RA-depleted graft. All patients experienced rapid donor engraftment, with median neutrophil engraftment on Day +11 (range: 10-12). At Day +30, the median T-cell count was 91.5 TCRγδ T-cells/µl and 263 CD45RO+ (memory) T-cells/µL (range 0-2,286; Table 1). The frequency of regulatory T-cells (Tregs) was significantly (p<0.05) increased at Day +30 in patients who received sirolimus, with a median concentration of 17 cell/µl (range 1-67), compared to patients treated with tacrolimus (median: 2.5 cell/µl; range: 1-13). Four of 5 patients, who received tacrolimus prophylaxis, developed Grade III-IV GVHD, all of which occurred after tacrolimus was stopped either as per protocol (Day +60; n=2) or due to drug-toxicity (n=2). To date, only 2 of 13 patients who received sirolimus prophylaxis have developed grade III-IV GVHD, with 10 patients being at least 100 days post haploHCT. Fourteen patients remain alive with a median follow up of 347 days (range 61-727). One patient died of treatment related causes (Day +370), and 3 patients died of progressive disease (Days +144, 233, and 321).
Conclusion: Our results indicate that TCRɑß- and CD45RA-depletion can be safely combined in the haploHCT setting, allowing for rapid engraftment and immune reconstitution, with a low incidence of aGVHD using sirolimus prophylaxis. Overall survival is encouraging (78%) at a median follow up of 11½ months in this high-risk population receiving 2nd/3rd allogeneic HCT, warranting further active exploration of our modified approach to haploHCT.
Triplett:Miltenyi Biotec: Other: Travel Support, to present previously published work at EBMT symposium.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal